The Connection Between Adrenochrome and the “Fight or Flight” Hormone
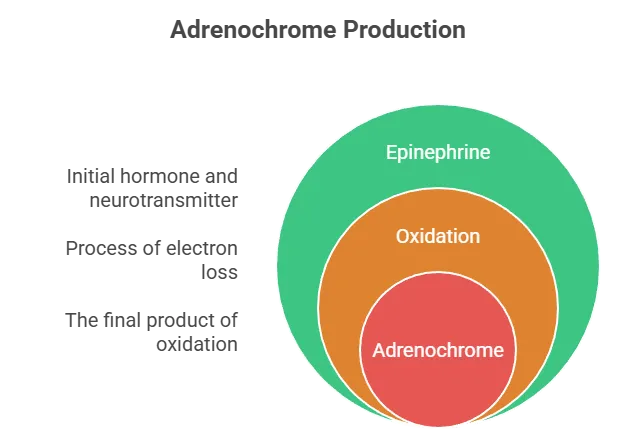
The “fight or flight” hormone refers to adrenaline (also known as epinephrine), a key stress hormone produced by the adrenal glands. It triggers the body’s rapid response to perceived threats, increasing heart rate, blood pressure, and energy mobilization. Adrenochrome is directly related to adrenaline, but it’s not the hormone itself—it’s a byproduct formed from adrenaline’s breakdown. Here’s a breakdown of the relationship:
- Research History: Early studies (1950s) by psychiatrists like Abram Hoffer investigated adrenochrome’s potential links to mental health, hypothesizing it might play a role in conditions like schizophrenia due to its oxidative properties. However, this was largely debunked, and modern science sees no such connection.
- Misconceptions: In conspiracy theories (e.g., QAnon), adrenochrome is falsely claimed to be harvested from adrenaline during torture for “euphoric” effects. This is baseless—adrenochrome isn’t a drug, and no evidence supports extraction or use in humans. It’s purely a biochemical curiosity.
Adrenochrome: Complete Medical FAQ
Evidence-based answers to 13 common questions about adrenochrome, separating scientific facts from popular myths. Click on any question to see the detailed medical explanation.
Adrenochrome (chemical formula: C₉H₉NO₃) is an organic compound that forms when adrenaline (epinephrine) undergoes oxidation. It was first identified in the 1950s and appears as a pink-to-orange colored compound in solution.
Key Chemical Properties:
- Molecular weight: 179.17 g/mol
- Formed via oxidation of adrenaline’s catechol ring structure
- Studied in laboratory settings as a research chemical
- Exists primarily as a metabolite in biochemical studies
From a pharmacological perspective, adrenochrome is classified as a laboratory reagent or research chemical. It has no approved medical applications in any healthcare system worldwide and is not manufactured as a pharmaceutical product.
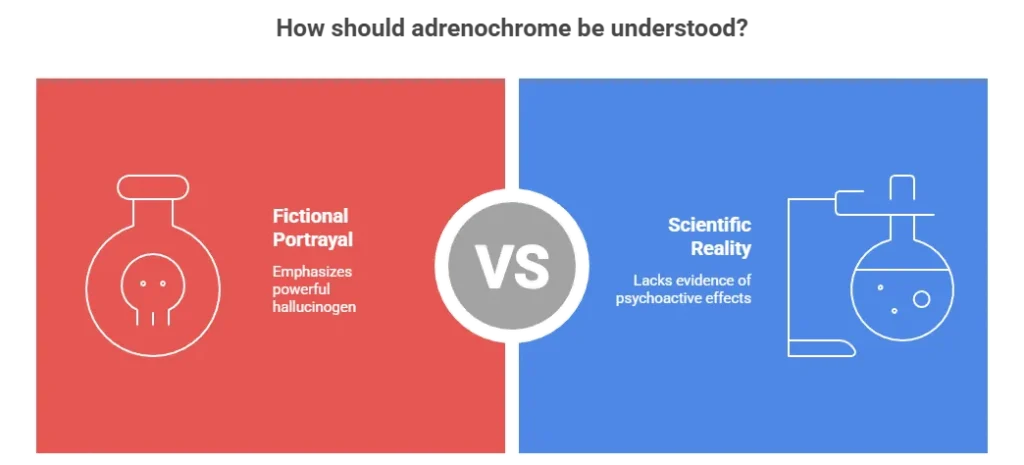
No, adrenochrome has no hallucinogenic properties and is not used as a recreational drug. This misconception represents one of the most persistent medical myths circulating online.
Origins of the Myth:
- 1950s-60s Speculation: A few poorly designed studies suggested possible psychological effects, but these were never replicated or validated
- Pop Culture Influence: Hunter S. Thompson’s 1971 book “Fear and Loathing in Las Vegas” fictionalized adrenochrome as a hallucinogen
- Internet Amplification: Online forums transformed fiction into “fact” through repetition without evidence
Pharmacological Reality: Modern neuroscience finds no evidence that adrenochrome interacts with serotonin, dopamine, or any neurotransmitter systems associated with psychoactive effects. It is chemically unrelated to known hallucinogens like LSD, psilocybin, or DMT.
This claim violates multiple principles of biochemistry, physiology, and basic mathematics. Here’s why it’s biologically impossible:
The Mathematical Reality:
The average human body contains approximately 0.01-0.03 micrograms of adrenaline per liter of blood. To produce just 1 milligram of adrenochrome would require processing:
30,000 – 100,000 liters of human blood
This equals the blood volume of 6,000-20,000 people – a logistically absurd proposition.
How It’s Actually Produced:
- All adrenochrome for research is synthesized from simple chemical precursors in laboratories
- Common starting materials include commercially available adrenaline bitartrate
- Synthesis costs pennies per gram compared to biological extraction
- The process involves simple oxidation reactions, not biological harvesting
No, adrenochrome has zero approved medical applications in any recognized medical system worldwide.
What Medical Databases Show:
- WHO: Not listed in Essential Medicines List
- FDA: No approved drug applications
- EMA: No marketing authorizations in Europe
- Pharmacopeias: Not included in USP, BP, or other pharmacopeias
- Clinical Trials: No ongoing trials on ClinicalTrials.gov
Complete Absence from Medicine: You will not find adrenochrome in:
- Hospital formularies or pharmacy inventories
- Medical textbook treatment protocols
- Physician prescription pads or electronic health records
- Medical insurance reimbursement codes
When mentioned in contemporary literature, adrenochrome appears only in toxicology studies, oxidative stress research, or methodological papers as a chemical reagent.
Known and Potential Risks:
- Cytotoxicity: Laboratory studies show it can be toxic to cells
- Oxidative Damage: May promote oxidative stress in biological systems
- Unknown Pharmacokinetics: How the body processes it is largely unstudied
- No Safety Profile: Established safe dosage levels don’t exist
- Impurity Risks: Illicit preparations may contain dangerous contaminants
Medical Advice: Ingesting or experimenting with adrenochrome is potentially dangerous and medically irresponsible. The absence of safety data means effects could range from mild toxicity to severe organ damage.
Major global health organizations have no official position on adrenochrome because it has no medical relevance or application in clinical practice.
WHO
No listing in Essential Medicines; no therapeutic recommendations
FDA
No approved applications; not recognized as a drug
EMA
No marketing authorizations; not in European pharmacopeia
CDC
No public health alerts or advisories regarding adrenochrome
Professional Medical Associations: Organizations like the AMA, BMA, and WMA have no guidelines, position statements, or educational materials about adrenochrome because it doesn’t exist in medical practice.
Claims that adrenochrome has anti-aging, youth-preserving, or longevity-extending properties are 100% fabricated with zero scientific basis.
Why These Claims Are Scientifically Absurd:
- No Mechanism: Adrenochrome has no known biological pathways that affect aging
- Contradictory Chemistry: As a potential pro-oxidant, it might accelerate cellular aging
- No Research: Zero studies show anti-aging effects in any organism
- Legitimate Gerontology: Aging research focuses on telomeres, senescent cells, mitochondrial function – not adrenochrome
Step-by-Step Response:
- Refuse Firmly: Clearly state “no” without engaging in debate
- Do Not Ingest: Under no circumstances consume the substance
- Secure Your Safety: Remove yourself from the situation
- Document Details: Note descriptions, locations, identifying information
- Report to Authorities: Contact local law enforcement
- Warn Others: Alert friends or community members
What You’re Likely Being Offered: Since genuine adrenochrome is essentially unavailable outside research labs, any substance offered as “adrenochrome” is almost certainly:
- A completely different (and potentially dangerous) chemical
- A placebo substance with unknown composition
- A fraudulent product with mislabeled ingredients
- An attempt to exploit conspiracy beliefs for financial gain
For accurate, evidence-based information about adrenochrome, consult these reliable sources:
Academic Databases
- PubMed/NCBI (National Center for Biotechnology Information)
- Google Scholar
- ScienceDirect
- JSTOR
Educational Institutions
- University pharmacology departments
- Toxicology research centers
- Medical school biochemistry programs
- Public health university resources
- Make extraordinary claims without peer-reviewed evidence
- Cite anonymous or unverifiable sources
- Use emotional language rather than scientific terminology
- Promote conspiracy theories over evidence
Absolutely not. This represents dangerous medical misinformation with no basis in reality.
Actual COVID-19 Vaccine Components:
- mRNA vaccines: Lipid nanoparticles containing mRNA instructions
- Viral vector vaccines: Modified adenoviruses carrying genetic material
- Protein subunit vaccines: Viral spike proteins
- Common excipients: Salts, sugars, lipids, buffers – standard pharmaceutical ingredients
No Scientific Connection: Adrenochrome is not used in vaccine development, production, or testing. This false connection has been repeatedly debunked by virologists, immunologists, and public health authorities worldwide.
Medical professionals dismiss adrenochrome claims because they:
- Lack scientific plausibility (violate basic pharmacology principles)
- Have zero empirical evidence (no clinical trials, case studies, or documented use)
- Promote potentially harmful behavior (encouraging use of toxic substances)
- Distract from legitimate health issues that need public attention
- Often accompany harmful conspiracy theories with real-world consequences
The Evidence Standard in Medicine:
Legitimate medical treatments require:
- Preclinical laboratory studies
- Phase I-III clinical trials
- Peer-reviewed publication
- Regulatory approval (FDA, EMA, etc.)
- Post-market surveillance
Adrenochrome has none of these evidence markers.
While science never says “never,” current evidence suggests adrenochrome is extremely unlikely to have future medical applications.
Current Research Landscape:
- No Active Research: No studies are investigating therapeutic uses
- Unpromising Chemistry: Its chemical properties don’t suggest medical potential
- Competition: Thousands of more promising compounds are being studied
- Safety Concerns: Initial studies suggest potential toxicity
What Future Use Would Require:
- Decades of preclinical research
- Multiple phases of clinical trials
- Regulatory approval processes
- Demonstration of safety and efficacy
- Cost-effectiveness compared to existing treatments
None of these processes are underway or planned for adrenochrome.
The overwhelming medical and scientific consensus is clear:
Adrenochrome is a laboratory research chemical with no medical significance.
It has no therapeutic applications, no recreational use, no anti-aging properties, and plays no role in medical practice or legitimate research beyond basic toxicology studies.
Summary of Key Facts:
- Chemical Status: Research compound, not a pharmaceutical drug
- Medical Status: No approved uses in any medical system
- Safety Status: Potentially toxic with unknown human effects
- Regulatory Status: Not controlled but also not approved
- Scientific Status: Mentioned only in limited laboratory research
What is Adrenaline (the Fight or Flight Hormone)?
- Role in the Body: Adrenaline is released during stressful situations (e.g., danger, exercise, or excitement) to prepare the body for action. It signals the sympathetic nervous system, leading to effects like dilated pupils, faster breathing, and heightened alertness.
- Production: Synthesized in the adrenal medulla from amino acids like tyrosine, via enzymes like phenylethanolamine N-methyltransferase (PNMT).
- Chemical Structure: It’s a catecholamine (C9H13NO3), a type of neurotransmitter and hormone.
What is Adrenochrome?
- Formation: Adrenochrome is an oxidation product of adrenaline. When adrenaline is exposed to oxygen or oxidizing agents (e.g., in the bloodstream or during metabolism), it undergoes a chemical reaction that converts it into adrenochrome (C9H9NO3), a red-colored quinone compound.
- Biological Context: This happens naturally in small amounts in the body, particularly in tissues like the adrenal glands and brain, where adrenaline is metabolized. It’s not produced intentionally but as a side effect of adrenaline’s instability.
- Stability and Effects: Adrenochrome is highly unstable and quickly degrades. In high concentrations (artificial or experimental), it can cause oxidative stress or mild neurological effects, but it has no significant role in normal physiology.
The Direct Link
- Metabolic Pathway: Adrenaline → Oxidation → Adrenochrome. Essentially, adrenochrome is what happens when adrenaline “ages” or reacts with oxygen. This process was first studied in the 1950s by researchers like Albert Szent-Györgyi, who explored oxidation in biological systems.
- Why It Matters: During intense fight or flight responses, adrenaline surges, and some of it may oxidize into adrenochrome. However, this is a minor, trace byproduct—most adrenaline is metabolized differently (e.g., via monoamine oxidase into other compounds like vanillylmandelic acid).
- No Functional Role in Fight or Flight: Adrenochrome doesn’t contribute to the fight or flight response; it’s just a metabolic dead-end. The core hormone driving that response is adrenaline itself.
Scientific and Historical Notes
Adrenaline: Mechanisms, Biochemistry, and Related Pathways
Adrenaline (epinephrine) is the primary “fight or flight” hormone, orchestrating the body’s rapid response to stress. Below, I’ll break down its mechanisms, biochemical production and metabolism, and connections to related compounds like adrenochrome. This is based on established endocrinology and neuroscience (e.g., sources like Guyton and Hall’s Textbook of Medical Physiology and PubMed studies).
Mechanisms of Action in Fight or Flight
Adrenaline prepares the body for immediate action by activating the sympathetic nervous system. Here’s how it works:
- Release Trigger: Stressors (e.g., fear, exercise, or hypoglycemia) signal the hypothalamus to activate the sympathetic nervous system, prompting the adrenal medulla to secrete adrenaline into the bloodstream. This happens within seconds.
- Physiological Effects:
- Cardiovascular: Increases heart rate and contractility, constricts blood vessels in non-essential areas (e.g., skin), and dilates vessels in muscles/skeletal tissues for better oxygen delivery.
- Respiratory: Bronchodilation (opens airways) for more oxygen intake.
- Metabolic: Stimulates glycogen breakdown in liver/muscles for quick energy (glucose release), inhibits insulin to maintain blood sugar.
- Neurological: Heightens alertness, focus, and pain tolerance via beta-adrenergic receptors in the brain.
- Other: Pupil dilation, reduced digestion, and increased sweating.
- Receptor Interactions: Adrenaline binds to adrenergic receptors (alpha and beta subtypes). Beta-2 receptors mediate most fight-or-flight effects, while alpha-1 causes vasoconstriction. This is why beta-blockers (e.g., propranolol) can blunt these responses.
- Duration: Effects peak in 1-2 minutes and last 5-10 minutes, as adrenaline is quickly metabolized or cleared.
Evidence: Studies like those in Nature Reviews Endocrinology (2018) confirm adrenaline’s role in acute stress responses, with measurable spikes in plasma levels during threats.
Biochemical Production and Metabolism
- Synthesis Pathway: Adrenaline is made from the amino acid tyrosine in the adrenal medulla:
- Tyrosine → L-DOPA (via tyrosine hydroxylase).
- L-DOPA → Dopamine (via aromatic L-amino acid decarboxylase).
- Dopamine → Norepinephrine (via dopamine beta-hydroxylase).
- Norepinephrine → Adrenaline (via phenylethanolamine N-methyltransferase, PNMT, which requires SAM as a methyl donor).
- Storage and Release: Stored in chromaffin granules in adrenal cells; released via exocytosis when stimulated by acetylcholine from sympathetic nerves.
- Metabolism and Breakdown:
- Primary Routes:
- Catechol-O-methyltransferase (COMT) and monoamine oxidase (MAO) enzymes degrade it into metabolites like metanephrine, vanillylmandelic acid (VMA), and normetanephrine, which are excreted in urine.
- In the liver and kidneys, it’s conjugated and cleared.
- Oxidation to Adrenochrome: A minor pathway occurs when adrenaline auto-oxidizes in the presence of oxygen or metal ions, forming adrenochrome (a red quinone). This is not enzymatic and happens in vitro or under oxidative stress, producing free radicals. Adrenochrome is unstable and further degrades; it’s not a functional metabolite but a byproduct (e.g., studied in 1950s for potential toxicity).
- Half-Life: About 2-3 minutes in plasma due to rapid uptake and metabolism.
- Primary Routes:
Evidence: Biochemical pathways are well-documented in textbooks like Biochemistry by Berg et al., with clinical assays (e.g., 24-hour urine VMA tests) used to diagnose adrenal tumors like pheochromocytoma.
Related Biochemistry and Disorders
- Similar Compounds: Adrenaline is part of the catecholamine family, alongside norepinephrine (noradrenaline, more involved in sustained stress) and dopamine. Norepinephrine is the precursor and has overlapping effects.
- Disorders: Excess adrenaline (e.g., in pheochromocytoma) causes hypertension and tachycardia. Deficiency (rare) leads to fatigue. Adrenaline autoimmunity (e.g., in some allergies) can trigger anaphylaxis.
- Therapeutic Uses: Synthetic adrenaline (epinephrine) is used in EpiPens for anaphylaxis, CPR, and asthma inhalers.
- Tie to Adrenochrome: As noted, adrenochrome forms from adrenaline oxidation, but it’s insignificant physiologically—high levels (e.g., in lab experiments) can cause oxidative damage, but no natural accumulation occurs. Conspiracy claims of “harvesting” it are debunked, as it’s not isolable in usable quantities from humans.
Norepinephrine: Biochemistry and Role in Stress Response
Norepinephrine (noradrenaline) is closely related to adrenaline but plays a distinct role in the body’s stress system. It’s both a neurotransmitter and a hormone, bridging the nervous and endocrine systems.
- Biochemical Production: Like adrenaline, it’s synthesized from tyrosine in the adrenal medulla and neurons:
- Tyrosine → L-DOPA → Dopamine → Norepinephrine (via dopamine beta-hydroxylase).
- In neurons, it’s stored in vesicles and released at synapses; in the adrenal glands, it’s converted to adrenaline by PNMT.
- Role in Fight or Flight:
- Neurotransmitter Function: Released from sympathetic nerve endings, it acts locally to maintain vascular tone, increase heart rate, and mobilize energy. It’s key for sustained arousal (e.g., during prolonged stress), unlike adrenaline’s rapid, systemic surge.
- Hormonal Function: Secreted from the adrenal medulla (about 20% of catecholamine output), it complements adrenaline by enhancing alertness, focus, and vasoconstriction. Effects include increased blood pressure, reduced blood flow to intestines, and heightened sensory perception.
- Comparison to Adrenaline: Adrenaline is more “episodic” (short bursts for immediate threats), while norepinephrine handles “tonic” stress (ongoing vigilance). Both bind adrenergic receptors, but norepinephrine prefers alpha receptors for constriction, adrenaline beta for dilation/relaxation.
- Metabolism: Broken down by COMT and MAO into metabolites like 3-methoxy-4-hydroxymandelic acid (MHMA). It can also oxidize to form compounds like noradrenochrome (similar to adrenochrome), but this is minor and not functional.
- Disorders and Effects: Imbalances link to anxiety, depression (low levels), or hypertension (high). Drugs like SSRIs affect norepinephrine reuptake.
Evidence: Studies (e.g., in Journal of Neuroscience, 2010) show norepinephrine’s role in cognitive stress responses, with PET scans revealing its release in the locus coeruleus during threats.
Clinical Tests for Adrenaline and Norepinephrine
Diagnosing issues with catecholamines (adrenaline/norepinephrine) involves measuring levels to detect tumors, deficiencies, or imbalances. These tests are crucial for conditions like pheochromocytoma (adrenal tumors causing excess secretion).
- Blood Tests: Plasma catecholamine assays measure free adrenaline/norepinephrine. Normal ranges: Adrenaline 10-100 pg/mL, Norepinephrine 100-500 pg/mL. Elevated levels indicate pheochromocytoma or stress disorders. Samples are drawn supine (resting) to avoid false positives from activity.
- Urine Tests: 24-hour urine collection for metabolites like vanillylmandelic acid (VMA), metanephrines, and normetanephrines. More reliable than blood for tumors, as it captures cumulative output. Normal: VMA <6.5 mg/24h. Used in screening for neuroblastoma or adrenal hyperplasia.
- Provocative Tests: Clonidine suppression test (for pheochromocytoma) or glucagon stimulation (to provoke secretion). Imaging (MRI/CT) confirms tumors.
- Other Diagnostics: Genetic testing for mutations (e.g., VHL gene in hereditary pheochromocytoma). In emergencies, like anaphylaxis, adrenaline levels aren’t routinely tested—treatment (EpiPen) is prioritized.
Evidence: Guidelines from the Endocrine Society (2022) recommend urine metanephrines as first-line for diagnosis, with sensitivity >95% for pheochromocytoma.
Evolutionary Aspects of Fight or Flight
The fight or flight response evolved as a survival mechanism in vertebrates, enhancing adaptability to threats. It’s rooted in the autonomic nervous system, which predates mammals.
- Origins: Traces back to early chordates (e.g., fish) with primitive sympathetic systems. In mammals, it developed via the hypothalamic-pituitary-adrenal (HPA) axis, integrating adrenaline/norepinephrine for rapid escape or confrontation. This likely evolved from ancestral “freeze” responses in invertebrates.
- Survival Benefits: Allows quick energy redirection (e.g., glucose for muscles) and heightened senses, improving predation avoidance or hunting success. In humans, it aids social threats (e.g., public speaking) but can maladapt in chronic stress, leading to diseases like heart disease.
- Evolutionary Trade-Offs: Short-term advantage (e.g., escaping predators) vs. long-term costs (e.g., cortisol release wears down immunity). Genetic variations (e.g., in COMT gene) influence response intensity, with “warrior” alleles linked to higher adrenaline in some populations.
- Modern Context: In urban settings, it’s triggered by non-physical threats (e.g., deadlines), potentially contributing to “modern stress syndrome.” Evolutionary psychology views it as a mismatch between ancestral environments (high physical danger) and today’s (psychological stress).
Evidence: Research in Evolutionary Psychology (2015) links catecholamine responses to ancestral survival, with fossil evidence of stress markers in dinosaurs suggesting ancient analogs.
Deeper Dive: Specific Disorders, Evolutionary Genetics, and Norepinephrine in Depression
Continuing from our discussion on adrenaline, norepinephrine, and fight or flight, I’ll expand on three key areas: specific disorders involving catecholamine imbalances, evolutionary genetics influencing these responses, and norepinephrine’s role in depression. This draws from clinical endocrinology, genetics, and psychiatry (e.g., sources like The Lancet and Nature Genetics).
Specific Disorders Involving Catecholamine Imbalances
Catecholamines like adrenaline and norepinephrine are central to stress responses, so disruptions can cause serious conditions. Here’s a breakdown of key disorders:
- Pheochromocytoma: A rare adrenal gland tumor (incidence ~0.8 per 100,000) that overproduces adrenaline and norepinephrine, leading to paroxysmal hypertension, headaches, sweating, and palpitations. It’s often hereditary (e.g., linked to RET or VHL genes). Diagnosis uses 24-hour urine metanephrines; treatment involves surgery or alpha-blockers like phenoxybenzamine. Untreated, it can cause heart failure or strokes.
- Adrenal Insufficiency (Addison’s Disease): Underproduction of cortisol and catecholamines due to adrenal gland damage (e.g., autoimmune, infection, or steroids). Symptoms include fatigue, hypotension, and poor stress response (no “fight or flight” surge). Blood tests show low cortisol; treatment is lifelong hydrocortisone replacement. Adrenaline deficiency is less critical but contributes to hypoglycemia.
- Catecholamine-Related Anxiety Disorders: Conditions like panic disorder or PTSD involve dysregulated norepinephrine release from the locus coeruleus, causing hyperarousal. Beta-blockers (e.g., propranolol) reduce symptoms by blocking adrenaline effects. Genetic factors (e.g., COMT variants) increase risk.
- Other: Neuroblastoma (childhood cancer) overproduces catecholamines, detectable via urine VMA. In diabetes, adrenaline surges can worsen hyperglycemia.
Evidence: Endocrine Society guidelines (2022) emphasize genetic screening for pheochromocytoma, with imaging confirming 90% of cases.
Evolutionary Genetics of Fight or Flight Responses
Genetic variations shape how individuals respond to stress, reflecting evolutionary adaptations for survival in ancestral environments (e.g., hunter-gatherer threats).
- Key Genes:
- COMT (Catechol-O-Methyltransferase): Encodes an enzyme that breaks down dopamine, norepinephrine, and adrenaline. The “Val158Met” polymorphism affects enzyme efficiency—Val carriers have faster breakdown, leading to lower catecholamine levels and better stress tolerance (e.g., in “warrior” populations). Met carriers may have higher anxiety but better cognition under stress. Evolutionary advantage: Val variant linked to risk-taking in harsh environments.
- ADRB2 (Beta-2 Adrenergic Receptor): Variants influence adrenaline binding. The Gly16Arg polymorphism affects receptor desensitization—Arg carriers show stronger fight-or-flight responses, potentially aiding quick escapes but increasing hypertension risk.
- PNMT (Phenylethanolamine N-Methyltransferase): Regulates adrenaline synthesis; variations correlate with stress resilience, with higher PNMT activity in populations adapted to cold climates (e.g., Inuit).
- Evolutionary Context: These genes show selection pressures from Pleistocene-era threats (e.g., predation). Modern mismatches (e.g., chronic urban stress) can exacerbate issues like heart disease in susceptible genotypes. Twin studies show 40-60% heritability for stress responses.
Evidence: GWAS studies (e.g., in PLoS Genetics, 2016) link COMT variants to stress phenotypes, with evolutionary models (e.g., via natural selection simulations) supporting adaptation.
Norepinephrine’s Role in Depression
Norepinephrine is implicated in mood regulation, particularly in depression, where imbalances contribute to symptoms like low energy and anhedonia.
- Mechanism: Norepinephrine modulates arousal and motivation via the locus coeruleus (brainstem nucleus). Low levels impair prefrontal cortex function, leading to executive dysfunction. It’s part of the monoamine hypothesis (alongside serotonin), where depression stems from neurotransmitter deficits.
- Role in Depression Subtypes: In melancholic or atypical depression, norepinephrine dysregulation causes fatigue and apathy. Chronic stress depletes it, creating a vicious cycle (e.g., via HPA axis overactivation).
- Treatments Targeting Norepinephrine: SNRIs (e.g., venlafaxine, duloxetine) inhibit reuptake, increasing synaptic norepinephrine. They are effective for treatment-resistant depression, with remission rates ~30-50% higher than SSRIs alone. Tricyclic antidepressants (e.g., desipramine) also boost norepinephrine.
- Evidence and Caveats: Meta-analyses (e.g., in JAMA Psychiatry, 2018) show SNRIs superior for severe depression. However, not all respond; genetics (e.g., NET gene variants) influence efficacy. Overstimulation can cause anxiety or insomnia.
The Role of Adrenochrome: Biological, Historical, and Cultural Perspectives
Adrenochrome, the oxidized byproduct of adrenaline (epinephrine), has been a subject of scientific curiosity, historical research, and modern misinformation. However, it plays no significant or essential role in human biology, physiology, or the fight or flight response. Below, I’ll break down its limited functions, historical context, and why it’s often misunderstood. This is grounded in biochemistry and endocrinology (e.g., from PubMed and historical studies like those by Abram Hoffer).
Biological Role
- Minimal Physiological Function: Adrenochrome is a trace metabolite formed when adrenaline oxidizes in the presence of oxygen or reactive species (e.g., in the adrenal glands, blood, or brain). It has no known vital role in normal human function—it’s not a hormone, neurotransmitter, or enzyme. Natural levels are negligible, and the body doesn’t produce or use it intentionally. Its instability (half-life of minutes) prevents accumulation or utility.
- Potential Effects in Excess: In high, artificial concentrations (e.g., lab-induced), it can act as a pro-oxidant, generating free radicals that cause oxidative stress or mild neurotoxicity. Early studies (1950s) noted it might induce hallucinations or psychotic symptoms in animal models, but this is not relevant to natural physiology. It doesn’t contribute to fight or flight; that’s adrenaline’s domain.
- Metabolic Pathway: Adrenaline → Oxidation → Adrenochrome → Further degradation (e.g., to melanin-like pigments). It’s a dead-end product, not recycled or utilized.
Evidence: Modern biochemistry (e.g., Biochemical Journal, 2000s) views it as an inert byproduct, with no essential pathways involving it.
Historical and Research Role
- Scientific Investigation: Discovered in 1952 by Albert Szent-Györgyi, it was studied for its role in oxidation processes and vitamin C metabolism. Psychiatrists like Hoffer hypothesized it might exacerbate schizophrenia by accumulating in the brain, leading to experiments with antioxidants (e.g., niacin) to counteract it. However, these ideas were discredited by the 1970s, as schizophrenia is now linked to genetics, neuroinflammation, and dopamine imbalances, not adrenochrome.
- Experimental Uses: Limited lab research explores its antioxidant/pro-oxidant duality (e.g., in redox studies), but it’s not pursued for therapeutics. No clinical trials or drugs involve it today.
- Toxicity Studies: Animal experiments showed high doses cause behavioral changes, but this is artifactual and not applicable to humans.
Role in Conspiracy Theories and Culture
- Pseudoscientific Claims: In fringe theories (e.g., QAnon), adrenochrome is falsely portrayed as a “youth elixir” or hallucinogen harvested from humans (allegedly via torture) for elite use. This stems from Hunter S. Thompson’s satirical novel Fear and Loathing in Las Vegas (1971), where it’s depicted as a fictional drug. No evidence supports extraction, effects, or harvesting—it’s a debunked myth promoting harm (e.g., threats against accused figures).
- Cultural Impact: It appears in media (e.g., Stranger Things, music lyrics) as a mysterious compound, fueling viral misinformation. Fact-checkers like Snopes emphasize its lack of real-world role.
Conclusion
Adrenochrome’s “role” is essentially nonexistent in biology—it’s a minor, unstable byproduct of adrenaline metabolism with no functional significance. Its prominence in conspiracies overshadows its scientific irrelevance. If you’re asking about its role in a specific context (e.g., oxidation chemistry or mental health theories), or want comparisons to other catecholamine byproducts, provide more details! For reliable info, check sources like NIH or PubMed.
Disclaimer: Medical and Scientific Information
The following text is presented to address public inquiries and clarify facts regarding the substance adrenochrome, as discussed in certain public forums. This information is based on established toxicological, pharmacological, and medical literature.
1. What is Adrenochrome?
Adrenochrome is a chemical compound produced by the oxidation of adrenaline (epinephrine). It is a real substance studied in laboratory settings since the mid-20th century. It has no approved medical use in humans.
2. Historical and Research Context
- In the 1950s and 1960s, some speculative research explored its potential psychological effects, leading to unfounded theories. These early studies were inconclusive, methodologically flawed by modern standards, and have not been substantiated by rigorous scientific research.
- Adrenochrome has been used in laboratory research as a reagent (e.g., in studies of oxidative stress or melanin synthesis). It is not a controlled or scheduled substance under major international drug control treaties.
3. Medical and Toxicological Facts
- No Therapeutic Value: Adrenochrome is not a pharmaceutical drug. It is not used in any standard, alternative, or experimental medical treatment for any condition.
- Potential Toxicity: Like many oxidation products, adrenochrome may be cytotoxic (toxic to cells). Ingesting or administering it is considered unsafe and poses health risks.
- Source Clarification: While it can be derived from adrenaline, which is produced by the human body and animals, the notion that it is “harvested” from human sources for any significant use is scientifically implausible and medically nonsensical. Synthesis in a laboratory from simple chemical precursors is the only practical method of obtaining it for research.
4. Correction of Misinformation
- Psychoactive “Drug”: Claims that adrenochrome is a potent hallucinogen or a secret youth-preserving elixir are entirely false and have no basis in pharmacology, neuroscience, or clinical medicine. They are considered baseless conspiracy theories.
- Criminal Allegations: Horrific narratives involving adrenochrome are categorically false, lack any credible evidence, and are often used to propagate hate and violence. Law enforcement agencies globally have found no evidence to support such claims.
5. Purpose of This Clarification
This document aims to provide clear, evidence-based facts to counteract widespread misinformation. Public interest appears to stem from fictional portrayals and online conspiracy theories, not from medical or scientific reality.
6. Important Public Health Warning
The public is strongly advised that adrenochrome is not a recreational drug. Seeking out, ingesting, or experimenting with this chemical is dangerous and poses a significant risk to health. It is an unapproved, unresearched chemical with unknown and potentially severe toxic effects.
Medical Information Disclaimer: Facts on Adrenochrome
Authored by: Dr. Mohammed Abdul Azeem Siddiqui
Purpose: To clarify scientific and medical facts and counteract public misinformation.
Contact for Document Clarification: powerofprevention@outlook.com
Remember: Your health is important. Always consult with a real-world healthcare provider for personal medical concerns.
Disclaimer: This document is for informational purposes only and is based on current, publicly available scientific and medical consensus. It does not constitute medical advice. For health concerns, always consult a qualified healthcare professional. The author disclaims any liability for actions taken based on the content of this informational note.
This response is for reference only.
